Functional abdominal bloating and distention (FABD) is one of the most commonly reported gastric issues to physicians. FABD may be thought of as a sole complaint or may coexist with other functional gastrointestinal disorders such as functional dyspepsia, irritable bowel syndrome, and functional constipation.
Bloating can be defined as a sense of gassiness or a sense of being distended; measurable distention does not have to occur, whereas abdominal distention should be reserved for patients who show a visible increase in abdominal girth.
About 30% of the general adult population report bloating and distention along with IBS. However, half of the people with bloating also report abdominal distention.1 It is noted that bloating is common among patients with IBS, whereas distention is more common in patients with chronic constipation.2
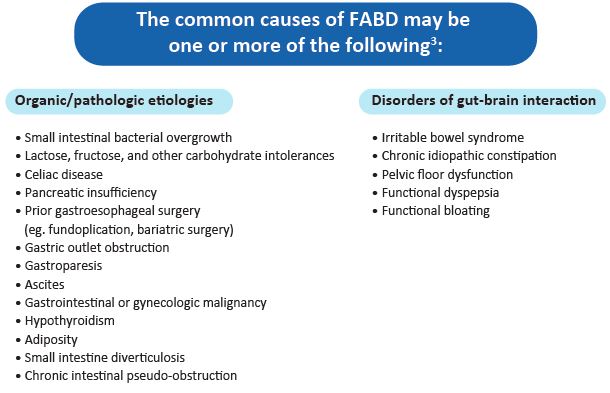
Common causative factors for FABD.
The aetiology of abdominal bloating and distention is multifactorial.
Although it is otien misunderstood that ‘gas’ in GI tract is the reason for bloating and distention, it is a causal agent in very few cases of FABD.
1) Increased Intraluminal Content
Intraluminal content includes water, air, gas, and faecal material. Air and gas may become copious within the lumen through aerophagia and potentially from the overproduction of gas by colonic or small intestine bacteria.4 Small intestinal bacterial overgrowth (SIBO), gas under-absorption, and diet high in fermentable, poorly digested and absorbed carbohydrates may all play a role in causing FABD.5
2) Visceral Hypersensitivity
Increased gut sensitivity and heightened attention to intraluminal contents may give rise to functional abdominal bloating and distention. Patients with IBS have a high awareness of their gut contents and motility and thus may experience even a slightly modified gut intraluminal content as bloating.6
Malagelada et al. used the term “conscious perception” to explain the role of the brain-gut axis in symptom generation (abdominal bloating). According to this model, visceral allodynia (seen also in IBS) is responsible for the bloating sensation that occurs in the presence of normal or only mildly increased amounts of intraluminal gas or other bowel content.7
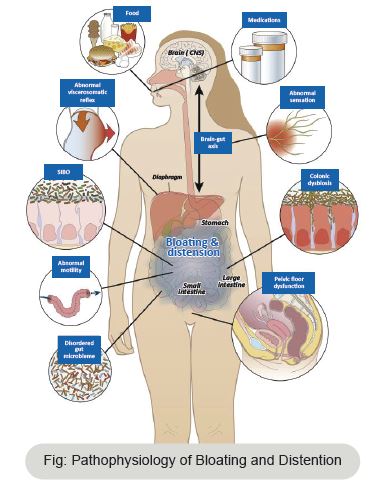
3) Abdomino-Phrenic Dyssynergia
Abdomino-Phrenic Dyssynergia is a term coined by the Barcelona group. It describes the responses of patients with FABD to a meal. According to the study by the same group,patients with FABD have a distinguished and abnormal muscle activity characterised by anterior abdominal wall relaxation and diaphragm contraction. This activity causes the abdominal gas to redistribute and cause an anterior wall protrusion with noticeable distention.8
4) Constipation and Outilow Obstruction
Functional abdominal bloating and distension may be related to constipation and to functional outilow obstruction. Retained stool in the rectum may cause impaired gas evacuation and slowing of intestinal transit. Compared with healthy volunteers, patients with FABD have a slower colonic transit.9
5) Obesity
Rapid weight gain and weight loss are associated with aggravation and improvement in bloating, respectively.10 In one study, recent weight gain coincided with new-onset bloating in 25% of the participants . A possible mechanism may involve an abnormal viscero-somatic reflex originating in the abdominal adipose issue which modulates the brain-gut axis, resulting in FABD.11
6) Dysbiosis
Aberrant constitution or alteration in colonic microbacteria may lead to increased production of colonic gas by fermentation or decreased gas consumption, leading to increased colonic gas content and bloating.12 Collins et al. observed that interruption of the host–microbiota equilibrium affects the intestinal immune system and leads to inflammation. This, in turn, leads to gut sensory and motor dysfunction which may contribute to bloating.13
More recently, Ringel-Kulka et al. studied the relationship between the intestinal microbiota, abdominal bloating, and altered bowel patterns in a cohort of patients with IBS and found significant changes in microbiota among different IBS subtypes. In particular, the authors noted that bloating was associated with specific microbial taxa.14
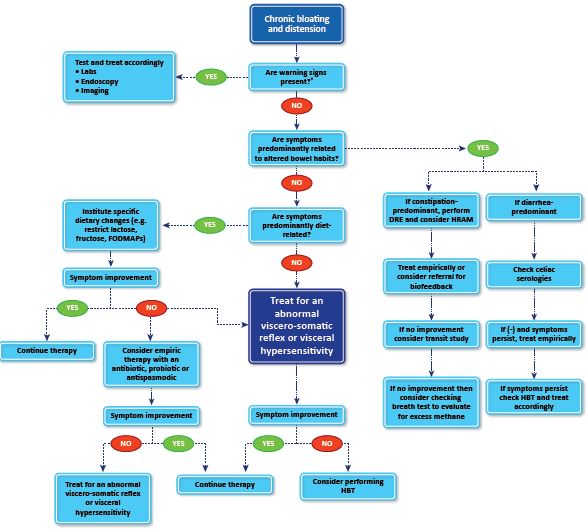
As the pathophysiology of FABD is multifactorial, the treatment of the FABD is also complex. The reason for FABD needs to be evaluated before one can start treating it.
Treatment options:
1) Symptomatic management: Antispasmodics and Simethicone can be used for symptomatic relief.
2) Dietary intervention: The main goal here is to understand the diet of the patient and what food items the patient is intolerant to. Restriction of lactose and poorly absorbed carbohydrates is usually one of the initial steps of dietary intervention.
3) Treatment of constipation: As in most cases, constipation could be the reason. Medications like Linaclotide and Pyridostigmine seem to help.
4) Microbiome modulation: Rifaximin and probiotics help in maintaining healthy gut microbiome.
5) Abdominal biofeedback therapy: Acting on the diaphragm and abdominal muscles, this therapy helps in treating FABD.16
Abdominal bloating and distention are very common issues which impose a lot of discomfort. Based on the various studies, the reasons that this happens could vary from simple dyspepsia to hypothyroidism. Hence, as the aetiology is multifactorial, the treatment also needs to have a different approach with one or more lines of management.
Reference:
1. Azpiroz F. Intestinal gas. In: Feldman M, Friedman LS, Brand LJ, editors. Pathophysiology, diagnosis, management. Philadelphia: Elsevier; 2015. p. 242–50.
2. Tuteja A, Talley N, Joos S, Tolman K, Hickam D. Abdominal bloating in employed adults: prevalence, risk factors, and association with other bowel disorders. Am J Gastroenterol. 2008;103(5):1241–8.
3. Lacy, Brian E., David Cangemi, and Maria Vazquez-Roque. "Management of chronic abdominal distension and bloating." Clinical Gastroenterology and Hepatology 19.2 (2021): 219-231.
4. Drossman D. Functional gastrointestinal disorders: history, pathophysiology, clinical features, and Rome IV. Gastroenterology. 2016;150(6):1262–79.
5. Chang L, Lee O, Naliboff B, Schmulson M, Mayer E. Sensation of bloating and visible abdominal distension in patients with irritable bowel syndrome. Am J Gastroenterol. 2001;96(12):3341–7.
6. Serra J, Azpiroz F, Malagelada J. Modulation of gut perception in humans by spatial summation phenomena. J Physiol. 1998;506(2):579–87.
7. Malagelada J, Accarino A, Azpiroz F. Bloating and abdominal distension: old misconceptions and current knowledge. Am J Gastroenterol. 2017;112(8):1221–31.
8. Chang, Lin, et al. "Sensation of bloating and visible abdominal distension in patients with irritable bowel syndrome." The American journal of gastroenterology 96.12 (2001): 3341-3347.
9. Talley, Nicholas J., et al. "Overlapping upper and lower gastrointestinal symptoms in irritable bowel syndrome patients with constipation or diarrhea." The American journal of gastroenterology 98.11 (2003): 2454-2459.
10. Malagelada J, Accarino A, Azpiroz F. Bloating and abdominal distension: old misconceptions and current knowledge. Am J Gastroenterol. 2017;112(8):1221–31.Agrawal A, Houghton L, Reilly B, Morris J, Whorwell P. Bloating and distension in irritable bowel syndrome: the role of gastrointestinal transit. Am J Gastro
11. Drossman D. Functional gastrointestinal disorders: history, pathophysiology, clinical features, and Rome IV. Gastroenterology. 2016;150(6):1262–79.
12. Simrén M, Barbara G, Flint H, et al. Intestinal microbiota in functional bowel disorders: a Rome Foundation report. Gut. 2012;62(1):159–76.
13. Collins S, Denou E, Verdu E, Bercik P. The putative role of the intestinal microbiota in the irritable bowel syndrome. Dig Liver Dis. 2009;41(12):850–3.
14. Ringel-Kulka T, Benson A, Carroll I, Kim J, Legge R, Ringel Y. Molecular characterization of the intestinal microbiota in patients with and without abdominal bloating. Am J Physiol Gastrointest Liver Physiol. 2016;310(6):G417–26.
15. Lacy, Brian E., David Cangemi, and Maria Vazquez-Roque. "Management of chronic abdominal distension and bloating." Clinical Gastroenterology and Hepatology 19.2 (2021): 219-231.
16. Mari, A., Abu Backer, F., Mahamid, M. et al. Bloating and Abdominal Distension: Clinical Approach and Management. Adv Ther 36, 1075–1084 (2019). https://doi.org/10.1007/s12325-019-00924-7
