Urinary Tract Infections (UTIs) are among the most widespread infections in clinical practice worldwide. With over 8.3 million clinic visits and more than 1 million hospitalizations, cases of UTI are both morbid and recurrent. A single type of bacteria, for example, E.coli causes about 80-90% of UTIs.
UTIs are more common in women than men. Around 50% of women experience Urinary tract infections (UTI) at some point in their lives which has been a growing cause of concern.1
Even though the prevalence data shows that the occurrence of UTI is most likely between the ages of 14 and 24, both men and women of older ages experience episodes of uncomplicated UTIs just as much. In men, symptomatic UTIs are less common with 12% prevalence rates.2

Increased, indiscriminate use or abuse of antibiotics may lead to antibiotic resistance. It occurs when bacteria develop the ability to survive exposure to antibiotics that are designed to inhibit or destroy them. These resistant bacteria continue to grow and multiply and become much more difficult to treat when resistance is developed. Increasing resistance is observed in the use of drugs like trimethoprim-sulfamethoxazole (TMP-SMZ) which are commonly employed as the first line of treatment for uncomplicated UTIs.
The resistance to uropathogenic Escherichia coli and treatment with TMP-SMZ lies in the range of 14.6% to 60%. Fluoroquinolone drugs like ciprofloxacin also seem to have increased resistance which is higher in developing countries (55.5-85.5%) than in developed countries.3 As resistance rates for standard antibiotics are increasing, so are the challenges for obtaining optimal efficacy in the treatment of UTIs. Also, there is a lack of empirical therapy in the current scenario. Studies by far have rarely quantified the risk factors on the overall susceptibility of standard empiric therapy choices.4 In most cases, the microbiological results are not available until 24 to 72 hours. In such cases, initial therapy is often empiric therapy and is guided by clinical presentations. A common approach that is sought is to use broad-spectrum antibiotics or sometimes a combination of antibiotics as initial empiric therapy. Empiric antibiotic therapy is important as it covers multiple possible pathogens that may be commonly associated with a specific clinical syndrome.
Clinicians should consider the following while selecting empiric antibiotic therapy:
● Prior knowledge of the bacteria that affects the patients
● The site of infection and the organism that likely colonised the site.
● The local bacterial resistance patterns that are available at the hospital or health centre.
Studies indicate that the resistance percentages of the causative organism should be below 20% to consider an agent suitable for empirical treatment of lower UTI and below 10% for upper UTI.
Owing to this, the resistance percentages of amoxicillin, TMP, and TMP-SMX are not suitable for the empirical treatment of pyelonephritis and other complicated UTIs as per the studies. Ciprofloxacin is usually recommended only when the treatment is given orally, when patients don't require hospitalization or when patients have anaphylaxis for beta-lactam antibiosis.
Also, ciprofloxacin and other fluoroquinolones are not suitable for empiric treatment of complicated UTIs in patients from the urology department or when they have been using fluoroquinolones in their last 6 months of treatment.
Data suggest that patients with UTI showing systemic symptoms requiring hospitalization should be treated with an aminoglycoside, preferably with second-generation cephalosporin.
A few studies also indicate that cephalosporin’s show promising potency against resistant strains and are effective in hospitalized patients, especially patients affected with upper UTIs.5
A comparative study showed that fluoroquinolones and third-generation cephalosporins differed in their resistance rates.With more than 25% difference, third-generation cephalosporin showed lower resistance rates indicating a promising treatment option.A comparison table with the number of resistant episodes to formulate the data in a research conducted is given below.
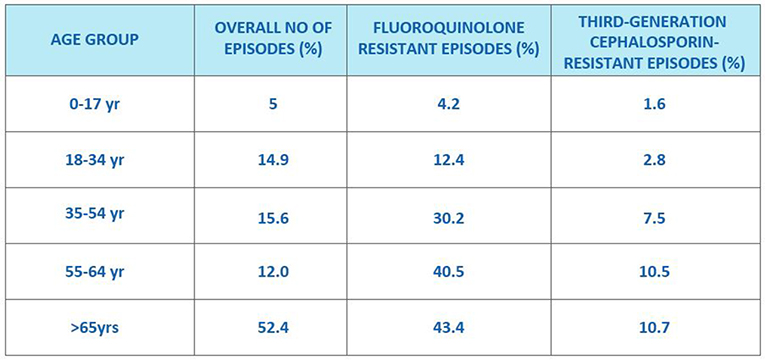
Currently, both fluoroquinolones antibiotics and third-generation cephalosporins are employed in the empirical treatment of UTI, but studies indicate that third-generation cephalosporins such as ceftriaxone and ceftazidime as empirical treatment for hospitalized patients with UTI should be preferred over fluoroquinolones.6 Evidence also suggests that a 2nd generation cephalosporin plus an aminoglycoside or a 3rd generation cephalosporin IV can be recommended as empirical treatment of complicated UTIs over other agents.
In many settings a 3rd generation cephalosporin without an aminoglycoside seems to be a good alternative, depending on the local resistance data and severity of patient symptoms or in case of community-onset complicated UTI. Evidence indicates that in events of hypersensitivity of penicillin, a 3rd generation cephalosporin can be prescribed, with an exception of beta-lactam antibiotics that have caused systemic anaphylaxis in the past. This is because; only a small chance of cross-hypersensitivity exists between penicillin derivatives and cephalosporins.7
Not one but multiple studies incline towards using cephalosporins over other drugs used in the treatment of UTIs because of lower resistance rates. Empirical treatment using cephalosporin seems to be the preferred choice in the effective antibiotic resistance treatment.
Reference:
1. Who.int. 2022. [online] Available at: <https://www.who.int/gpsc/information_centre/cauda-uti_eccmid.pdf>
2. Medina, M. and Castillo-Pino, E., 2019. An introduction to the epidemiology and burden of urinary tract infections. Therapeutic Advances in Urology, 11, p.175628721983217.
3. KOT, B., 2019. Antibiotic Resistance Among Uropathogenic Escherichia coli. Polish Journal of Microbiology, 68(4), pp.403-415.
4. Bischoff, S., Walter, T., Gerigk, M., Ebert, M. and Vogelmann, R., 2018. Empiric antibiotic therapy in urinary tract infection in patients with risk factors for antibiotic resistance in a German emergency department. BMC Infectious Diseases, 18(1).
5. Gentry, L., 1987. Cephalosporins in Urinary Tract Infection. Drugs, 34(Supplement 2), pp.154-163.
6. Bidell, M., Palchak, M., Mohr, J. and Lodise, T., 2016. Fluoroquinolone and Third-Generation-Cephalosporin Resistance among Hospitalized Patients with Urinary Tract Infections Due to Escherichia coli: Do Rates Vary by Hospital Characteristics and Geographic Region?. Antimicrobial Agents and Chemotherapy, 60(5), pp.3170-3173.
7. Chaudhry, S., Veve, M. and Wagner, J., 2022. Cephalosporins: A Focus on Side Chains and β-Lactam Cross-Reactivity.
